Can these new studies offer hope for people with lung and head and neck cancers?

Two new studies enrolling patients at Providence Cancer Institute of Oregon may offer hope to people with KRAS G12C-mutant non-small cell lung cancer, and head and neck squamous cell carcinoma. Read on to find out how the outcomes from these studies may fill critical gaps in treatment options.
New targeted therapy evaluated for treating NSCLC with KRAS G12C
 A new study for people with a specific type of lung cancer, called KRAS G12C-mutant non-small cell lung cancer (NSCLC), is open for enrollment at Providence Cancer Institute. Study JZQB, also known as SUNRAY-01, is an important global clinical trial testing a new drug combination for treating NSCLC with the KRAS G12C mutation that is advanced and cannot be surgically removed.
A new study for people with a specific type of lung cancer, called KRAS G12C-mutant non-small cell lung cancer (NSCLC), is open for enrollment at Providence Cancer Institute. Study JZQB, also known as SUNRAY-01, is an important global clinical trial testing a new drug combination for treating NSCLC with the KRAS G12C mutation that is advanced and cannot be surgically removed.
This study aims to find the best way to use the new medication LY3537982 (also known as olomorasib), with either the combination of chemotherapy and the immunotherapy pembrolizumab, or with pembrolizumab alone. LY3537982 targets the mutated KRAS G12C protein. It works by binding to the mutated protein and keeping it in an inactive state.
Why treating KRAS mutations in NSCLC is difficult
Lung cancer causes the most cancer-related deaths worldwide each year. NSCLC makes up 80-90% of lung cancer cases, and most patients are diagnosed at an advanced stage, when surgery is not an option and the disease is not curable at that point.
Current treatments for NSCLC without specific genetic targets often include immune checkpoint inhibitors (immunotherapy), either alone or with platinum-based chemotherapy. However, for NSCLC patients with specific genetic mutations, targeted therapies can be effective at controlling the cancer, as well.
KRAS mutations are common in NSCLC, and about 12% of these involve the KRAS G12C mutation. Currently, there are targeted therapies approved for treating NSCLC with KRAS G12C mutations, but with chemotherapy.
This study is looking at a new targeted therapy as part of the combination as a first-line therapy for this disease.
Two-part study evaluates therapeutic combinations
SUNRAY-01 has two main parts:
- In Part A, approximately 384 participants will be randomly assigned to receive either the LY3537982 and pembrolizumab combination or the placebo and pembrolizumab combination.
- In Part B, around 552 participants will receive either the LY3537982 combination with pembrolizumab, pemetrexed and platinum or the placebo with these medications.
Before starting these comparisons, the study will determine the best dose of LY3537982 to use. This will be done by looking at data from an earlier study (LOXO-RAS-20001) and from initial testing within the current study. This is called “Dose Optimization and Safety Lead-In phases.” For this study, Dose Optimization, Part A and Part B are randomized. Safety Lead-In for Part B is single arm, non-randomized.
Get more information about this study:
The principal investigator of this study is Rachel Sanborn, M.D., medical director, Providence Thoracic Oncology Program and the Phase I Clinical Trials Program at Providence Cancer Institute.
Can volrustomig help reduce the risk of cancer recurrence in people with locally advanced HNSCC?
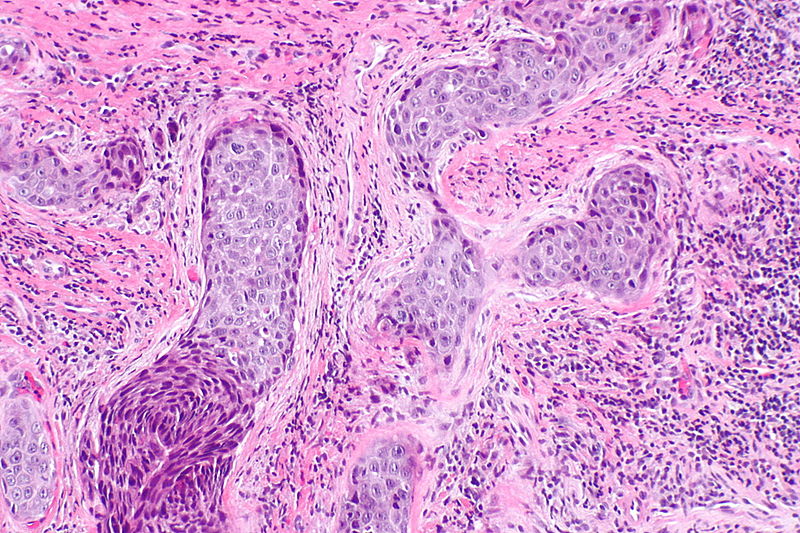
Over 60% of people with head and neck squamous cell carcinoma (HNSCC) are diagnosed at a locally advanced stage, where the cancer has not yet spread to distant parts of the body but remains challenging to treat.
For these people, the standard treatment usually involves a combination of radiation and chemotherapy, sometimes with surgery. Despite these efforts, outcomes can be poor.
A new clinical trial currently open and enrolling patients at Providence Cancer Institute is designed to evaluate the effectiveness and safety of a new immunotherapy medication called volrustomig in treating patients with locally advanced HNSCC. Patients will receive definitive treatment with combined chemoradiation, followed by volrustomig IV infusion, every three weeks for one year (treatment arm), or careful monitoring (control arm), which is standard of care. Definitive treatment means the plan for treating a disease or disorder has been chosen as the best one for a patient after all other choices have been considered.
In this phase III trial, participants will be randomly assigned 1:1 (50/50, like the flip of a coin) to either of the two arms.
HNSCC diagnoses in adults age 50+
Head and neck cancers account for nearly 4% of all cancers in the United States, according to the National Cancer Institute, and it’s more than twice as common in men than in women. The risk of developing HNSCC increases with age – the median age at diagnosis is 66 years for those with HPV-negative HNSCC and 53 years for those with HPV-positive HNSCC.
Recently, HPV infection has been identified as a major cause of HNSCC, especially in oropharyngeal cancer, which is more common in younger men. Genetic mutations also play a role in the development of HNSCC. For example, mutations in the TP53 gene are found in 72% of tumors, while mutations in CDKN2A and PIK3CA genes are also common.
The most common risk factors for all subtypes of HNSCC are tobacco and alcohol use. Other risk factors include exposure to radiation, poor oral hygiene, poor nutrition, chronic infections, long-term immunosuppression and infections with viruses like HPV and Epstein-Barr. Candida albicans infections also are linked to this type of cancer.
Does volrustomig show promise?
Volrustomig is being studied as a potential treatment for patients with unresected, locally advanced HNSCC who have already undergone chemoradiotherapy. The medication works by targeting and inhibiting specific proteins—PD-L1 and CTLA-4—that help tumors evade the immune system. This approach is already showing promise in treating recurrent and metastatic forms of the disease.
Researchers are now exploring its effectiveness in earlier stages. Immunotherapy following chemoradiation has already shown great promise, and it has been FDA approved as standard of care in other cancers like lung and esophageal cancers.
Two-arm trial design
The trial will involve around 1,145 participants who will be randomly assigned to one of two groups.
- Volrustomig Group (Arm A): Participants in this group will receive volrustomig through an IV infusion every 21 days for up to 12 months or 18 cycles. The treatment will continue unless the disease progresses based on specific medical criteria, if there are serious side effects, or if the participant chooses to stop.
- Observation Group (Arm B): Participants in this group will not receive the drug but will be closely monitored for up to 12 months. They will undergo regular medical assessments to check if the disease progresses or other conditions require discontinuation.
The study will also look at the impact of other factors like the presence of a protein called PD-L1, the site of the tumor, and whether the cancer is HPV-related. The study aims to see if volrustomig can help reduce the risk of cancer recurrence, compared to those who are simply observed.
The results will help determine whether volrustomig could become a new treatment, offering hope for people who currently have limited treatment options.
The principal investigator at Providence Cancer Institute is Rom Leidner, M.D., medical oncologist and director of Immune Cell Experimental Therapy, Earle A. Chiles Research Institute, a division of Providence Cancer Institute.
Refer a patient
To learn more or refer a patient to one of these clinical trials, contact our clinical research office:
- Call 503-215-1979
- Send an email
New research studies are added frequently. To see more clinical studies, visit:
- Studies for lung cancer
- Studies for oral, head and neck cancer
- All cancer studies at Providence Cancer Institute



